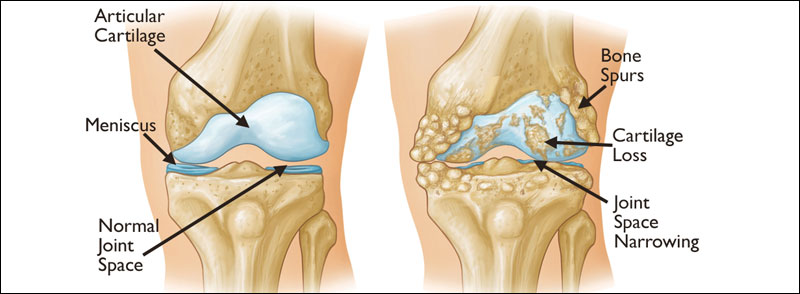
Osteoarthritis is a condition characterised by the World Health Organisation as the deterioration of cartilage in joints which results in bones rubbing together and creating stiffness, pain, and impaired movement. The degeneration and loss of cartilage can subsequently lead to alterations of the subchondral (underneath cartilage) bone. It is a reasonably common condition, 80% of adults over 50 will demonstrate some evidence of OA, which many people associated with wear and tear, as it is correlated with advancing age and excess pressure on joints.
However, it is slightly misleading to consider it a condition of wear and tear as this would suggest that the less you use your joints the less likely you are to develop osteoarthritis, this is not the case as sedentary lifestyle is a risk factor for the development of the condition. This blog will highlight the cause and drivers of osteoarthritis with interventions for protection against and support for those with this debilitating condition.1
Osteoarthritis is divided into two categories: primary and secondary.
Primary-:is the form more associated with wear and tear and aging, this degeneration process tends to occur at the age of 50-60, with no predisposing abnormalities. These changes are due to cumulative effects of decades of use leading to stress on the collagen matrix of cartilage. This damage causes the release of enzymes which destroy collagen components. On top of that, as we age our ability to synthesise and restore normal collagen structure decreases.
Secondary-:as the name suggests means that OA occurs in association with a predisposing factor that has caused degenerative changes. These include.
- Congenital abnormalities, such as hypermobility and abnormal joint structure
- Trauma (Joint injury but also includes obesity and surgeries)
- Crystal deposition (e.g., uric acid in gout)
- Prescence of abnormal cartilage (genetic)
- Inflammation (especially previous inflammatory disease such as rheumatoid arthritis)
Interventions to Support Osteoarthritis:
Repair of collagen matrix and regeneration of connective tissue cells
Cartilage is made up of specialised cells known as chondrocytes, these produce an extracellular matrix made up of collagen, proteoglycans, and elastin. This matrix acts as shock absorber in the joint, to take strain off the end of the bone and help prevent wear and tear on the cartilage itself. Therefore, supporting this matrix and regenerating chondrocytes is essential for supporting joint health.
Collagen –: Collagen type II is a major component of the extracellular matrix of hyaline cartilage and its synthesis and catabolism is regulated by chondrocytes (cells found in cartilage connective tissue).
Collagen type II fibres: the main structural component of cartilage, providing structure, firmness, and resistance to compression – account for 60% of cartilage. Studies have demonstrated that the supplementation of specific collagen peptides in young adults with functional knee problems led to a statistically significant improvement of activity-related joint pain.
Vitamin C–: vitamin C is essential to produce collagen, it is a cofactor in the binding, cross-linking, and folding of collagen to provide its unique structure. Several in vitro studies have shown that vitamin C has an anabolic effect on cartilage. A threefold reduction in the risk of OA progression was found in the middle and highest tertials of vitamin C intake. Additionally, there is evidence that vitamin C is useful for pain relief particularly of the musculoskeletal system, and vitamin C deficiency is associated with higher incidence of pain. Accumulating evidence indicates that vitamin C can exhibit analgesic properties in some clinical conditions, thus potentially mitigating suffering and improving patient quality of life
Glycosaminoglycans (GAGs)-: mainly consist of two building blocks – aggrecan (a large proteoglycan containing chondroitin sulphate) and hyaluronic acid, both essential components for maintaining a cushioned and lubricated joint environment, allowing for easy joint movement – this accounts for approximately 40% of the cartilage.
Hyaluronic Acid –: is another GAG in joints which provide a structural framework and allows cartilage to hold water. By the age of 70, hyaluronic acid contents has dropped by 80% leading to loss of connective tissue integrity, there by affecting joint health.
Glucosamine –: composed of a glucose and an amine molecule it has been shown to stimulate the production of glycosaminoglycans (GAGs), which give the shock absorbing capabilities of cartilage. It also promotes the incorporation of sulphur into cartilage. Studies show that the ability to manufacture glucosamine declines with age, therefore cartilage loses its shock-absorbing and gel-like functions, affecting the health of the joint and contributing to the progression of OA. Studies have shown reduced pain and improved quality of life in patients with OA
Bridge the nutrition gap Other nutrients including vitamins A, D and E, B6, zinc, copper and boron are all essential for collagen production. A deficiency in any one of these nutrients will contribute to accelerated joint degeneration. Therefore, it is recommended to use a multi vitamin and mineral to ensure optimal intake of all nutrients.
Reduce inflammation Inflammation plays a major role in osteoarthritis by contributing to both joint pain and degradation of the joint, therefore interventions to reduce inflammation are essential for supporting wellbeing of OA patients.
Reduce inflammation Inflammation plays a major role in osteoarthritis by contributing to both joint pain and degradation of the joint, therefore interventions to reduce inflammation are essential for supporting wellbeing of OA patients.
Boswellia-: is an Ayruvedic herb with anti-inflammatory properties. These anti-inflammatory effects have been investigated for their benefits in osteoarthritis (OA), and it appears that oral Boswellia supplements can suppress pain and immobility associated with OA quite significantly with the effects taking as little as a week to occur. (Examine.com). as well as reducing inflammation it is thought that Boswellia’s mechanism of action on joints also includes the prevention of GAG degradation and improved blood supply to joint tissues.
Proteolytic enzymes –: taken away from food, to simply prevent the breakdown of dietary protein, has been shown to reduce inflammatory markers including IL-6 and CRP5. Studies performed with bromelain (a proteolytic enzyme from pineapple) demonstrated as reduction in pain, swelling and joint stiffness in OA patients.
Celadrin-: Celadrin® is a patented combination of fatty acids which beneficially enhance the integrity of cell membranes in the body thus, subduing the inflammatory process and reducing pain. Hence Celadrin® is considered an aid to joint mobility and flexibility. It has high affinity for small joints, such as fingers. It is a combination of plant based fatty acids including cetyl myristoleate, cetyl palmiotoleate, cethy laureate, cetyl palmitate and cetyl oleate. Evidence shows that these fatty acids stabilise and enhance the integrity of cell membrane and therefore halts the production of inflamamtory compounds. It has also been shown to reduce the production of inflammatory markers including IL-6. It has been shown to improve knee range of motion, flexion and overall joint function in OA patients compared with placebo
Other interventions to reduce inflammation include:
- Reducing foods high in omega 6 – e.g., farmed meats, dairy products and vegetable oils (such as sunflower and corn oils). These are high in the omega 6 fat Arachidonic acid or Linoleic Acid (precursor to arachidonic acid). Arachidonic acid can be converted to the pro-inflammatory prostaglandin PGE
- Increasing sources of omega 3 from e.g., oily fish and flax, chia seeds and/or a supplement containing EPA. EPA is found in oily fish or can be supplemented; alpha linolenic acid is found in flax and chia seeds and dark leafy green vegetables and can be converted to EPA by the body. EPA is converted into anti-inflammatory prostaglandins.
- The ratio of omega 6 to 3 is very important, most people are consuming too high a level of omega 6 to 3 and therefore are often producing excess amounts of pro-inflammatory prostaglandins.
- Curcumin – found in turmeric, has been shown to inhibit Cox-2 enzymes which produce inflammatory prostaglandins.
- Obtaining good levels of vegetables (6-8 per day) including dark leafy greens high in anti-inflammatory phytonutrients and antioxidants.
- Vitamin E has been shown to supress inflammatory markers (IL-6, TNFα and NO) and down regulate the transcription factor NF-kB. Sources of Vitamin E are avocados, almonds, green vegetables, and olives.
